Table of Contents
Painkillers: Your First Step
Painkillers is a universal human experience, and finding the right way to manage it can make all the difference in your daily life. Whether it’s a sudden headache, chronic joint pain, or post-surgery discomfort, painkillers are often the first line of defense. But with so many options on the market, it’s important to understand what painkillers are, how they work, and when to use them safely.
Painkillers, also known as analgesics, are medicines designed to reduce or eliminate pain. They work by interrupting the pain signals in your nervous system or by reducing inflammation that causes discomfort. Different types of painkillers are used depending on the source and severity of the pain—ranging from mild over-the-counter options to stronger prescription medications. Choosing the right painkiller involves more than just grabbing a pill; it requires knowing the risks, benefits, and how they affect your body.
This guide will walk you through the most powerful and commonly used painkillers available today, helping you take control of pain management with confidence and clarity.
1. Tramadol: Painkiller for Moderate Pain Relief
Overview
Tramadol is a synthetic painkiller that mimics the effects of opioids and is commonly prescribed for managing moderate to moderately severe pain. It works by influencing the central nervous system to change how your brain interprets pain signals, providing fast relief for stubborn discomfort.
Primary Uses
- Post-operative pain management
- Chronic conditions such as lower back or joint pain
- Recovery from physical injuries
Possible Side Effects
- Drowsiness or dizziness, especially in older adults
- Nausea or constipation
- Risk of dependence or tolerance if used over a long period
Note: Tramadol is classified as a controlled substance in many countries due to its opioid-like action. Use this painkiller under strict medical supervision.
2. Celecoxib: A Targeted Painkiller Stomach Issues
Overview
Celecoxib belongs to a special group of NSAIDs called COX-2 inhibitors. Unlike traditional NSAIDs, this painkiller is designed to reduce inflammation and pain without causing major gastrointestinal distress, making it a preferred option for people with sensitive stomachs.
Primary Uses
- Managing osteoarthritis or rheumatoid arthritis pain
- Relief from painful menstrual cramps
- Inflammation-related joint stiffness
Possible Side Effects
- Slight risk of heart-related issues with long-term use
- Mild stomach discomfort (though less common than with regular NSAIDs)
- Headache or swelling in rare cases
Pro Tip: Celecoxib provides long-term relief for chronic conditions and is considered a safer NSAID for those prone to stomach ulcers.
3. Methadone: A Dual-Function Painkiller for Chronic Pain and Addiction Therapy
Overview
Methadone is a potent, long-acting opioid painkiller primarily used to manage severe chronic pain and assist in opioid addiction treatment. It modifies how the brain and spinal cord respond to pain, making it effective for conditions that other opioids may not fully control.
Primary Uses
- Chronic pain unresponsive to other painkillers
- Maintenance therapy for opioid addiction recovery programs
Possible Side Effects
- Respiratory suppression if dosage is too high
- Risk of serious overdose due to its long half-life
- Dizziness, confusion, or low blood pressure
Warning: Methadone must be administered carefully, often in a supervised medical setting, due to its strong effect and long duration in the body.

4. Tapentadol: A Dual-Action Painkiller
Overview
Tapentadol tablets is a centrally acting prescription painkiller that combines two powerful mechanisms: opioid receptor activation and norepinephrine reuptake inhibition. This unique combination allows it to control pain effectively while potentially causing fewer side effects than traditional opioids.
Common Uses
- Diabetic neuropathy
- Long-term musculoskeletal pain
- Pain management in patients intolerant to other opioids
Possible Side Effects
- Mild to moderate nausea
- Drowsiness or fatigue
- Risk of dependency with long-term or unsupervised use
Expert Tip: Among newer painkillers, Tapentadol stands out for treating nerve pain without the strong sedation that comes with older opioids.
5. Ketorolac: A Potent NSAID Painkiller for Short-Term Relief
Overview
Ketorolac is a high-strength nonsteroidal anti-inflammatory drug (NSAID) available only by prescription. It’s primarily used for short-term pain relief and is known for being as effective as mild opioids for certain conditions.
Common Uses
- Post-operative pain control
- Acute migraine attacks
- Relief from kidney stone pain
Possible Side Effects
- Gastrointestinal bleeding or ulcers
- Kidney function suppression
- Not recommended beyond 5 days of use
Caution: Although non-opioid, this painkiller must be used cautiously due to its high risk of gastrointestinal and renal complications.
6. Buprenorphine: A Long-Lasting Painkiller
Overview
Buprenorphine is a partial opioid agonist often prescribed for long-lasting pain relief in cases of severe or cancer-related discomfort. It’s available in patch or sublingual form, delivering steady pain control over time.
Common Uses
- Chronic severe pain, including in terminal illness
- Pain management for patients in opioid recovery programs
Possible Side Effects
- Sedation or dizziness
- Constipation
- Withdrawal symptoms if stopped abruptly
Note: Buprenorphine is one of the few painkillers that also plays a dual role in both pain control and addiction treatment.
7. Etoricoxib: A Gentle Yet Effective Painkiller
Overview
Etoricoxib is a selective COX-2 inhibitor designed to ease pain and inflammation while minimizing gastric side effects common with traditional NSAIDs. It’s favored for long-term use in inflammatory conditions.
Common Uses
- Gout attacks
- Osteoarthritis and rheumatoid arthritis
- Chronic back and neck pain
Possible Side Effects
- Water retention or ankle swelling
- Elevated blood pressure over time
Why It’s Popular: As a newer generation painkiller, Etoricoxib offers lasting relief with fewer stomach issues, making it ideal for patients with joint problems.
8. Diclofenac: A Trusted and Versatile Painkiller for Inflammation and Injury
Overview
Diclofenac is a widely used NSAID available in tablets, injections, and topical gels. Known for its anti-inflammatory strength, it’s often used for injury-related pain and chronic joint conditions.
Common Uses
- Sprains, strains, and sports injuries
- Arthritis-related joint stiffness and swelling
- Dental pain and inflammation
Possible Side Effects
- Stomach irritation or ulcers (oral form)
- Skin rash or redness (topical form)
Quick Fact: Diclofenac is one of the most prescribed painkillers globally due to its reliability and flexibility in treating a wide range of pain types.
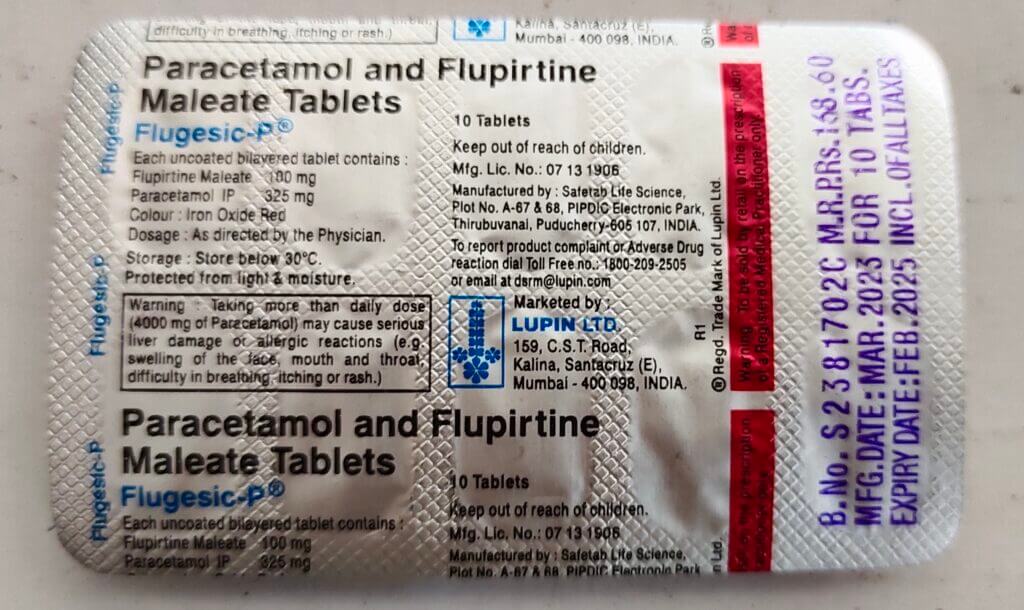
9. Flupirtine: A Banned Painkiller
Overview
Flupirtine was a non-opioid, non-NSAID painkiller known for its muscle-relaxant and neuroprotective properties. It was once prescribed for both acute and chronic pain conditions. However, due to its strong link with liver toxicity, many countries have banned or severely restricted its use.
Common Uses
- Lower back and spinal pain
- Orthopedic injuries
- Migraine episodes
Side Effects
- Severe liver damage with prolonged use
- Excessive fatigue
- Lightheadedness or dizziness
Important Note: Due to safety concerns, Flupirtine is no longer considered a viable painkiller in most regions. Always check current medical guidelines in your country.
10. Nefopam: A Non-Opioid Alternative
Overview
Nefopam is a unique non-opioid analgesic that offers pain relief without the gastrointestinal issues of NSAIDs or the dependency risks of opioids. Its mechanism is unrelated to commonly used painkillers, making it an option for patients who cannot tolerate traditional treatments.
Common Uses
- Surgical pain recovery
- Muscle and joint pain in sensitive patients
Side Effects
- Nausea or vomiting
- Anxiety or restlessness
- Increased sweating
Why It Matters: Nefopam serves as a useful alternative painkiller for individuals with contraindications to opioids or NSAIDs.
11. NSAIDs (Nonsteroidal Anti-Inflammatory Drugs)
Overview
NSAIDs are among the most frequently used over-the-counter painkillers. They work by blocking COX enzymes that promote inflammation, pain, and fever. NSAIDs are effective for both acute pain and ongoing conditions like arthritis.
Popular NSAIDs Include:
- Ibuprofen (Advil, Motrin)
- Naproxen (Aleve)
- Aspirin
Common Uses
- Joint inflammation (arthritis)
- Menstrual cramps
- Muscle aches and strains
- Fever and headaches
Risks and Side Effects
- Stomach ulcers or bleeding
- Kidney impairment
- Higher risk of heart attack or stroke with long-term use
Pro Tip: While NSAIDs are trusted painkillers, long-term use should always be monitored by a healthcare provider.
12. Acetaminophen (Paracetamol)
Overview
Acetaminophen, also known as paracetamol, is a go-to over-the-counter painkiller for mild to moderate pain. Unlike NSAIDs, it doesn’t reduce inflammation but is effective for fever and general discomfort.
Common Uses
- Headaches and migraines
- Low-grade fevers
- Minor body aches and flu symptoms
Risks and Side Effects
- Liver toxicity when taken in high doses or combined with alcohol
- Usually well-tolerated when used correctly
Good to Know: This widely available painkiller is safe for most people when taken within the recommended limits — always read the label.
13. Opioids: Powerful Painkillers for SevereConditions
Overview
Opioids are potent prescription-only painkillers used when other medications fail to provide relief. They alter the brain’s perception of pain and are effective for intense pain caused by surgery, injury, or cancer.
Common Opioids Include:
- Morphine
- Oxycodone (OxyContin)
- Hydrocodone (Vicodin)
- Fentanyl
- Codeine
Common Uses
- Post-operative recovery
- Cancer-related pain management
- Severe trauma or accident injuries
Risks and Side Effects
- High risk of addiction and tolerance
- Respiratory depression
- Constipation and digestive issues
- Drowsiness or confusion
Warning: Opioids are among the strongest painkillers available — use only under strict medical supervision to avoid complications.
14. Topical Painkillers
Overview
Topical analgesics are painkillers applied directly to the skin to relieve localized discomfort. They work at the site of pain and are ideal for those looking to avoid oral medications.
Popular Types Include:
- Capsaicin cream (derived from chili peppers)
- Lidocaine patches (numbing agent)
- Diclofenac gel (anti-inflammatory)
Common Uses
- Arthritis and joint stiffness
- Muscle soreness and tension
- Neuropathic (nerve-related) pain
Risks and Side Effects
- Skin irritation or redness
- Rare allergic reactions
Bonus Tip: These painkillers are great for targeted relief — perfect for those with sensitive stomachs or liver issues.

15. Antidepressants and Anticonvulsants
Overview
While traditionally used for depression and seizures, certain antidepressants and anticonvulsants have proven highly effective in managing chronic nerve pain. These medications help calm overactive pain signals in the nervous system.
Common Medications
- Amitriptyline – a tricyclic antidepressant
- Gabapentin – commonly used for nerve-related pain
- Pregabalin – a newer generation anticonvulsant
Effective For:
- Diabetic neuropathy
- Fibromyalgia
- Nerve pain after shingles (postherpetic neuralgia)
Risks and Side Effects
- Drowsiness and sedation
- Dizziness or balance issues
- Possible weight gain over time
Pro Tip: These drugs are often part of a comprehensive treatment plan for chronic pain sufferers who don’t find relief with standard painkillers.
16. Muscle Relaxants: Fast Relief for Muscle
Overview
Muscle relaxants are prescribed for short-term relief of acute muscle spasms or long-term muscle stiffness caused by neurological conditions. They work by calming nerve activity in the spinal cord.
Common Muscle Relaxants Include:
- Cyclobenzaprine – often used for back pain
- Methocarbamol – less sedating option
- Baclofen – ideal for spasticity from conditions like MS
Used For:
- Lower back pain or neck strain
- Muscle injuries or cramps
- Neurological disorders causing muscle tightness
Risks and Side Effects
- Sleepiness or grogginess
- Dizziness
- Dry mouth or fatigue
Helpful Hint: Best used for short-term issues or under close medical supervision for chronic conditions.
17. Corticosteroids: Powerful Inflammation Fighters
Overview
Corticosteroids are synthetic drugs that mimic cortisol — your body’s natural anti-inflammatory hormone. They’re often prescribed to quickly reduce swelling, inflammation, and pain from autoimmune or allergic conditions.
Common Corticosteroids
- Prednisone – commonly used orally
- Dexamethasone – often given in hospitals
Used To Treat:
- Rheumatoid arthritis and lupus
- Severe allergic reactions
- Chronic inflammatory conditions
Side Effects and Risks
- Fluid retention and weight gain
- Weakening of bones (osteoporosis)
- Elevated blood sugar and blood pressure
- Increased susceptibility to infections
Quick Note: Corticosteroids are incredibly effective painkillers when inflammation is the root cause, but long-term use should be carefully monitored.
18. NMDA Receptor Antagonists
Overview
NMDA receptor antagonists are a modern class of painkillers that block specific receptors in the brain and spinal cord involved in pain perception. They are particularly useful for complex or treatment-resistant pain.
Key Drugs
- Ketamine – used under medical supervision, often in hospitals
- Dextromethorphan – found in some cough suppressants and experimental pain therapies
Conditions Treated
- Chronic or neuropathic pain
- Post-surgical pain
- Complex regional pain syndrome (CRPS)
Risks and Side Effects
- Hallucinations or vivid dreams (especially with ketamine)
- Rise in blood pressure or heart rate
- Nausea or dizziness
Good to Know: NMDA antagonists are promising painkillers for those who haven’t responded to traditional therapies — but they must be used under strict medical care.
19. Cannabinoids
Overview
Cannabinoids are compounds derived from cannabis that interact with the body’s endocannabinoid system to regulate pain, inflammation, and mood. They’re gaining popularity as alternative painkillers, especially for chronic and neuropathic conditions.
Key Cannabinoids
- THC (Tetrahydrocannabinol) – psychoactive and pain-relieving
- CBD (Cannabidiol) – non-psychoactive, anti-inflammatory
Helpful For:
- Chronic nerve pain
- Cancer-related pain
- Pain linked to inflammation or muscle spasms
Risks and Side Effects
- Drowsiness or brain fog
- Dry mouth
- Feeling “high” (with THC-containing products)
Legal Note: Availability and legality vary by country or state. Always consult your healthcare provider before using cannabinoid-based painkillers.

20. Over-the-Counter (OTC) Painkillers
Overview
OTC painkillers are among the most widely used medications for pain relief, offering a convenient solution for managing everyday discomforts without the need for a doctor’s prescription. They’re ideal for mild to moderate pain and are readily available at pharmacies and supermarkets.
Common OTC Painkillers
- Acetaminophen (Paracetamol) – effective for reducing pain and fever
- Ibuprofen – a nonsteroidal anti-inflammatory drug (NSAID) helpful for inflammation
- Aspirin – offers pain relief along with blood-thinning properties
Best For:
- Tension headaches and migraines
- Minor muscle aches or strains
- Menstrual cramps
- Fever and flu symptoms
Risks and Side Effects
While generally safe, misuse of OTC painkillers can lead to serious health problems:
- Acetaminophen: Risk of liver damage if taken in high doses
- Ibuprofen and Aspirin: May cause stomach irritation, ulcers, or kidney issues
- Always follow dosage instructions and consult a doctor if you have pre-existing conditions
Choosing the Right Painkiller: A Personalized Approach
Not all painkillers work the same for everyone. Selecting the right one requires a thoughtful assessment of:
- Type of pain: Is it acute (short-term) or chronic (long-term)?
- Pain origin: Inflammatory (like arthritis) vs. neuropathic (nerve-related)
- Your health status: Conditions like kidney disease, ulcers, or risk of addiction must be considered
- Other medications: Always be aware of potential interactions with current prescriptions or supplements
Beyond Pills: Non-Drug Alternatives for Pain Relief
In many cases, combining medications with non-pharmacological strategies offers superior pain relief. Here are some proven methods:
- Physical therapy: Strengthens muscles and improves mobility to reduce pain
- Cognitive-behavioral therapy (CBT): Helps manage chronic pain by changing pain-related thoughts and behaviors
- Acupuncture: This ancient practice may stimulate nerve points and reduce discomfort
- Mindfulness, meditation, and relaxation: Lowers stress, which can significantly reduce pain perception
FAQs About Painkillers
Q1: Can I take NSAIDs and acetaminophen together?
A: Yes, you can usually combine NSAIDs like ibuprofen with acetaminophen, as they work through different mechanisms. This combination can offer stronger pain relief, but it’s essential to follow proper dosing and consult a healthcare provider to avoid liver or kidney strain.
Q2: Are opioids safe for long-term pain relief?
A: Opioids can manage severe pain effectively in the short term. However, long-term use carries risks of tolerance, dependence, and addiction. Continuous supervision by a doctor is necessary if opioids are prescribed for chronic conditions.
Q3: What is considered the safest over-the-counter painkiller?
A: Acetaminophen is often regarded as the safest option for short-term pain relief, especially for people with sensitive stomachs. However, it must be used within recommended limits to prevent liver damage.
Q4: Can I use topical painkillers with oral medications?
A: Yes, combining a topical painkiller like diclofenac gel with oral medication can enhance pain relief. Just ensure they don’t contain the same active ingredient to avoid overdose.
Q5: Are there natural remedies that work like painkillers?
A: Yes, methods like acupuncture, yoga, massage, turmeric, and omega-3 supplements can relieve certain types of pain. Discuss these with your doctor to ensure they complement your current treatment.
Q6: How can I choose the right painkiller for my condition?
A: It depends on the nature, intensity, and cause of your pain. Short-term injuries may need NSAIDs, while nerve pain may respond better to antidepressants or anticonvulsants. A doctor can help match the best painkiller to your needs.
Q7: Can using painkillers lead to addiction?
A: Some painkillers, especially opioids, have a high potential for dependence if misused or taken long-term. Always use pain medication exactly as prescribed and report any concerns to your healthcare provider.
Q8: What should I do if I have side effects from painkillers?
A: Discontinue use and contact your healthcare provider immediately. Depending on the reaction, they may suggest a different painkiller or adjust your dosage.
Q9: Are painkillers safe to take during pregnancy?
A: Not all painkillers are safe for pregnant women. For example, ibuprofen is generally avoided during late pregnancy. Always consult your OB-GYN before using any pain medication while pregnant.
Q10: How quickly do painkillers start working?
A: Most oral painkillers like acetaminophen or ibuprofen start working within 30 to 60 minutes. Stronger medications, such as opioids, may have a varied onset depending on the form and dose.
Q11: Can children take the same painkillers as adults?
A: Children require different dosages and formulations. Some OTC painkillers like acetaminophen or ibuprofen are safe when dosed appropriately for their weight and age. Always check with a pediatrician first.
Q12: What’s the difference between managing acute and chronic pain?
A: Acute pain, often due to injury or surgery, usually resolves quickly and responds well to short-term use of painkillers. Chronic pain is ongoing and may require a long-term strategy involving both medications and non-drug therapies.
Q13: Should I eat before taking painkillers?
A: Some painkillers, particularly NSAIDs, should be taken with food to reduce the risk of stomach irritation or ulcers. Always read the label or ask your doctor for guidance.
Q14: Can I drink alcohol while using painkillers?
A: It’s best to avoid alcohol while taking painkillers, especially opioids or acetaminophen. Combining them can increase the risk of liver damage, drowsiness, or dangerous interactions.
Q15: How should painkillers be stored at home?
A: Store all medications in a cool, dry place away from direct sunlight. Keep them out of reach of children and pets, and never use expired medications. Proper disposal is also important for safety.
Q16: What are the warning signs of a painkiller overdose?
A: Symptoms may include confusion, extreme drowsiness, slow breathing, nausea, vomiting, and unresponsiveness. Seek emergency medical help if an overdose is suspected.
Q17: Can painkillers interact with other medications?
A: Yes. Painkillers can interact with drugs like blood thinners, antidepressants, or anti-seizure meds, potentially increasing side effects. Always inform your doctor of all medications and supplements you’re taking.
Q18: How are prescription painkillers different from OTC options?
A: OTC painkillers are intended for mild to moderate, short-term pain. Prescription medications are usually stronger, used for severe or chronic pain, and must be taken under medical guidance.
Q19: Do painkillers affect mood or mental health?
A: Some painkillers, especially opioids, may influence mood—causing euphoria, anxiety, or depression. Others, like antidepressants prescribed for pain, can also affect emotional balance. Always monitor your mental state and inform your provider of any changes.
Q20: What if I miss a dose of my prescription painkiller?
A: Take it as soon as you remember, unless it’s almost time for the next dose. Never double the dose to catch up. If unsure, consult your doctor or pharmacist for advice.






You helped me a lot with this post. http://www.kayswell.com I love the subject and I hope you continue to write excellent articles like this.
I have learn some just right stuff here. Certainly value bookmarking for revisiting. I surprise how much attempt you place to create this type of fantastic informative web site.
May I have information on the topic of your article? http://www.kayswell.com
Great beat ! I would like to apprentice while you amend your web site, http://www.kayswell.com how could i subscribe for a blog site? The account helped me a acceptable deal. I had been a little bit acquainted of this your broadcast provided bright clear concept
Thank you for your articles. I find them very helpful. Could you help me with something? http://www.kayswell.com
You’ve been great to me. Thank you! http://www.kayswell.com
Great beat ! I would like to apprentice while you amend your web site, http://www.kayswell.com how could i subscribe for a blog site? The account helped me a acceptable deal. I had been a little bit acquainted of this your broadcast provided bright clear concept
I want to thank you for your assistance and this post. It’s been great. http://www.kayswell.com
You helped me a lot with this post. http://www.kayswell.com I love the subject and I hope you continue to write excellent articles like this.
Good web site! I truly love how it is easy on my eyes and the data are well written. http://www.kayswell.com I am wondering how I could be notified whenever a new post has been made. I’ve subscribed to your RSS which must do the trick! Have a nice day!
You helped me a lot by posting this article and I love what I’m learning. http://www.kayswell.com
Very nice post. I just stumbled upon your weblog and wished to say that I’ve really enjoyed browsing your blog posts. After all I’ll be subscribing to your feed and I hope you write again soon!
The articles you write help me a lot and I like the topic http://www.kayswell.com
Appreciation to my father who informed me on the topic of this web site, this website is really amazing.
Good post however , I was wanting to know if you could write a litte more on this topic? I’d be very thankful if you could elaborate a little bit more. Thank you! http://www.kayswell.com
Wow, fantastic blog layout! How long have you been blogging for? you make blogging look easy. http://www.kayswell.com The overall look of your site is great, let alone the content!
Hello there! I could have sworn I’ve been to this blog before but after checking through some of the post I realized it’s new to me.Anyways, I’m definitely glad I found it and I’ll be bookmarking and checking back frequently! http://www.kayswell.com
to this require a great deal of work? I have very little knowledge of computer programming however I had been hoping to start my own blog in the near future. Anyway, should you have any suggestions or tips for new blog owners please share. http://www.kayswell.com I understand this is off topic but I simply needed to ask.
I am regular reader, how are you everybody? This post posted at this web page is genuinely pleasant. http://www.kayswell.com
Howdy just wanted to give you a quick heads up. The words in your article seem to be running off the screen in Ie. http://www.kayswell.com
Have you ever considered about including a little bit more than just your articles? I mean, what you say is fundamental and all. However imagine if you added some great images or video clips to give your posts more, “pop”! Your content is excellent but with images and clips, http://www.kayswell.com this website could undeniably be one of the best in its field.
This piece of writing will help the internet visitors for creating new web site or even a blog from start to end. http://www.kayswell.com
Superb post however , I was wanting to know if you could write a litte more on this subject? I’d be very grateful if you could elaborate a little bit further. http://www.kayswell.com
This paragraph will assist the internet users for building up new web site or even a blog from start to end. http://www.kayswell.com
This is a topic that’s near to my heart… Many thanks! http://www.kayswell.com Where are your contact details though?
Hi there to all, for the reason that I am truly keen of reading this website’s post to be updated daily. It carries fastidious data. http://www.kayswell.com
Hello my loved one! I wish to say that this post is amazing, great written and include approximately all significant infos. I would like to peer extra posts like this . http://www.kayswell.com
Hi there to every one, since I am really eager of reading this blog’s post to be updated on a regular basis. It includes fastidious data. http://www.kayswell.com
Wow, marvelous weblog structure! How long have you ever been running a blog for? you make running a blog glance easy. The overall look of your web site is wonderful, as smartly as the content material! http://www.kayswell.com
It’s amazing to pay a quick visit this web page and reading the views of all colleagues concerning this article, while I am also keen of getting familiarity. http://www.kayswell.com
Hello! I just wanted to ask if you ever have any problems with hackers? My last blog (wordpress) was hacked and I ended up losing months of hard work due to no back up. Do you have any methods to prevent hackers? http://www.kayswell.com
Great post. I was checking constantly this blog and I’m impressed! Extremely helpful info specially the last part 🙂 I care for such info a lot. I was seeking this certain information for a long time. Thank you and good luck.
This is my first time visit at here and i am actually happy to read everthing at alone place. http://www.kayswell.com
Its like you read my mind! You appear to know so much about this, like you wrote the book in it or something. http://www.kayswell.com
Hello mates, nice article and fastidious urging commented here, I am actually enjoying by these. http://www.kayswell.com
I’ve been surfing online more than 3 hours today, yet I never found any interesting article like yours. It’s pretty worth enough for me. Personally, if all webmasters and bloggers made good content as you did, the web will be much more useful than ever before.
Hello just wanted to give you a brief heads up and let you know a few of the images aren’t loading correctly. I’m not sure why but I think its a linking issue. I’ve tried it in two different internet browsers and both show the same results. http://www.kayswell.com
Hello my family member! I want to say that this post is amazing, great written and come with almost all significant infos. I would like to look more posts like this. http://www.kayswell.com
Pretty! This has been an incredibly wonderful post. Thank you for providing this information.
Hello my loved one! I wish to say that this post is amazing, great written and include approximately all significant infos. I would like to peer extra posts like this . http://www.kayswell.com
Hello mates, its wonderful post on the topic of cultureand entirely explained, keep it up all the time. http://www.kayswell.com
I feel this is one of the such a lot important information for me. And i’m satisfied reading your article. But should observation on some normal issues, The site style is perfect, the articles is actually nice :
I am curious to find out what blog platform you happen to be utilizing? I’m experiencing some minor security issues with my latest blog and I would like to find something more safeguarded. Do you have any suggestions? http://www.kayswell.com
Hello there, You’ve done a great job. I will definitely digg it and personally recommend to my friends. I am confident they will be benefited from this website. http://www.kayswell.com
You should be a part of a contest for one of the finest blogs on the net. I’m going to highly recommend this blog! http://www.kayswell.com
Hello mates, its wonderful post on the topic of cultureand entirely explained, keep it up all the time. http://www.kayswell.com
Touche. Outstanding arguments. Keep up the great work. http://www.kayswell.com
Hi there, its fastidious article concerning media print, we all be aware of media is a great source of data. http://www.kayswell.com
I like the valuable info you provide to your articles. I will bookmark your weblog and check once more here regularly. I am reasonably sure I’ll be told lots of new stuff proper right here! Best of luck for the following! http://www.kayswell.com
What’s Going down i’m new to this, I stumbled upon this I have discovered It absolutely useful and it has aided me out loads. I am hoping to give a contribution & assist other users like its helped me. http://www.kayswell.com Great job.
Sweet blog! I found it while searching on Yahoo News. Do you have any tips on how to get listed in Yahoo News?I’ve been trying for a while but I never seem to get there! Many thanks http://www.kayswell.com
It’s in point of fact a great and useful piece of info.I am glad that you just shared this useful info with us.Please keep us informed like this. Thanks for sharing. http://www.hairstylesvip.com
You’re so interesting! I don’t suppose I have read something like this before. So nice to discover another person with a few genuine thoughts on this subject. Seriously.. many thanks for starting this up. This web site is something that’s needed on the web, someone with a little originality! http://www.kayswell.com
I am not sure where you are getting your info, but good topic. I needs to spend some time learning more or understanding more. Thanks for excellent info I was looking for this information for my mission. http://www.kayswell.com
These are actually great ideas in about blogging. You have touched some pleasant things here. Any way keep up wrinting. http://www.kayswell.com
What’s up i am kavin, its my first time to commenting anywhere, when i read this paragraph i thought i could also make comment due to this sensible post. http://www.kayswell.com
What i do not understood is actually how you’re no longer really much more well-preferred than you may be now. You’re very intelligent. You know thus significantly in terms of this subject, made me personally believe it from a lot of numerous angles. http://www.ifashionstyles.com Its like men and women aren’t interested unless it’s something to do with Girl gaga! Your individual stuffs great. At all times deal with it up!
Oh my goodness! Incredible article dude! Many thanks, However I am experiencing problems with your RSS. I don’t understand the reason why I cannot join it. Is there anybody having the same RSS issues? Anyone that knows the solution will you kindly respond? Thanx!! http://www.kayswell.com
I’m extremely impressed with your writing skills as well as with the layout on your weblog. Is this a paid theme or did you customize it yourself? Anyway keep up the excellent quality writing,it is rare to see a nice blog like this one today. http://www.kayswell.com
Hello there, You’ve done a great job. I will certainly digg it and personally recommend to my friends. I’m sure they will be benefited from this site. http://www.kayswell.com
Great post. I was checking constantly this blog and I am impressed! Extremely useful information specifically the last part 🙂 I care for such information a lot. I was seeking this certain info for a long time. Thank you and good luck. http://www.kayswell.com
I really like what you guys tend to be up too. This kind of clever work and reporting! Keep up the amazing works guys I’ve added you guys to my blogroll. http://www.kayswell.com
I loved as much as you will receive carried out right here. The sketch is tasteful, your authored material stylish. nonetheless, you command get bought an edginess over that you wish be delivering the following. http://www.kayswell.com unwell unquestionably come further formerly again since exactly the same nearly very often inside case you shield this hike.
Your mode of explaining everything in this piece of writing is genuinely pleasant, every one be capable of simply be aware of it, Thanks a lot. http://www.kayswell.com
I really like what you guys tend to be up too. This kind of clever work and reporting! Keep up the amazing works guys I’ve added you guys to my blogroll. http://www.kayswell.com
Hurrah! In the end I got a weblog from where I know how to truly take helpful information regarding my study and knowledge. http://www.ifashionstyles.com
This is a topic that’s near to my heart… Many thanks! http://www.kayswell.com Where are your contact details though?
I’m really enjoying the design and layout of your website.It’s a very easy on the eyes which makes it much more pleasant for me to come here and visit more often. Did you hire out a developer to create your theme? http://www.kayswell.com
Wonderful goods from you, man. I’ve understand your stuff previous to and you’re just too excellent.I really like what you have acquired here, certainly likewhat you are stating and the way in which you say it.You make it entertaining and you still care for to keep it wise.I cant wait to read much more from you. http://www.kayswell.com This is actually a wonderful site.
Way cool! Some extremely valid points! I appreciate you penning this write-up and also the rest of the website is really good. http://www.kayswell.com
Sweet blog! I found it while searching on Yahoo News. Do you have any tips on how to get listed in Yahoo News?I’ve been trying for a while but I never seem to get there! Many thanks http://www.kayswell.com
Thanks for one’s marvelous posting! I truly enjoyed reading it, you are a great author.I will ensure that I bookmark your blog and will often come back in the future. http://www.kayswell.com I want to encourage you to definitely continue your great posts, have a nice day!
Hello! I just wanted to ask if you ever have any problems with hackers? My last blog (wordpress) was hacked and I ended up losing months of hard work due to no back up. Do you have any methods to prevent hackers? http://www.kayswell.com
You should be a part of a contest for one of the finest blogs on the net. I’m going to highly recommend this blog! http://www.kayswell.com
Hello colleagues, its enormous article regarding cultureand completely defined, keep it up all the time. http://www.kayswell.com
When I initially commented I clicked the “Notify me when new comments are added” checkbox and now each time a comment is added I get several emails with the same comment. Is there any way you can remove people from that service? Many thanks! http://www.kayswell.com
It’s genuinely very difficult in this busy life to listen news on Television, so I just use world wide web for that reason, and take the most up-to-date news. http://www.kayswell.com
What a information of un-ambiguity and preserveness of valuable familiarity on the topic of unexpected feelings. http://www.kayswell.com
If you would like to obtain a great deal from this paragraph then you have to apply these methods to your won website. http://www.kayswell.com
You actually make it seem so easy with your presentation but I find this matter to be actually something that I think I would never understand. It seems too complex and very broad for me. I’m looking forward for your next post, I will try to get the hang of it! http://www.kayswell.com
Thanks for one’s marvelous posting! I truly enjoyed reading it, you are a great author.I will ensure that I bookmark your blog and will often come back in the future. http://www.kayswell.com I want to encourage you to definitely continue your great posts, have a nice day!
I’m not sure where you’re getting your info, but great topic. I needs to spend some time learning more or understanding more. Thanks for great info I was looking for this information for my mission.
Somebody essentially assist to make critically posts I would state. That is the first time I frequented your website page and to this point? I amazed with the research you made to make this actual put up amazing. Magnificent task!
This is a topic that’s near to my heart… Many thanks! Where are your contact details though?
Appreciation to my father who informed me on the topic of this web site, this website is really amazing.
Hi there, everything is going sound here and ofcourse every one is sharing data, that’s really good, keep up writing. http://www.kayswell.com
Ahaa, its pleasant dialogue on the topic of this piece of writing here at this web site, I have read all that,so at this time me also commenting at this place. http://www.kayswell.com
This is a topic that’s near to my heart… Many thanks! http://www.kayswell.com Where are your contact details though?
Hi, Neat post. There is a problem with your site in web explorer, might test this? IE still is the market chief and a large component of other people will leave out your wonderful writing because of this problem.
You’re so interesting! I don’t suppose I have read something like this before. So nice to discover another person with a few genuine thoughts on this subject. Seriously.. many thanks for starting this up. This web site is something that’s needed on the web, someone with a little originality! http://www.kayswell.com
I’m curious to find out what blog system you have been using? I’m experiencing some small security issues with my latest blog and I’d like to find something more safe. Do you have any suggestions?
Do you mind if I quote a few of your articles as long as I provide credit and sources back to your website? My blog site is in the exact same area of interest as yours and my visitors would really benefit from a lot of the information you provide here.Please let me know if this ok with you. Regards!
Greate article. Keep posting such kind of info on your site. Im really impressed by your site. Hi there, You have done an excellent job. I’ll definitely digg it and individually suggest to my friends. I am sure they will be benefited from this web site. http://www.kayswell.com
Hello, i read your blog occasionally and i own a similar one and i was just curious if you get a lot of spam feedback? If so how do you stop it, any plugin or anything you can recommend? I get so much lately it’s driving me insane so any help is very much appreciated. http://www.kayswell.com
Hello, I enjoy reading through your article. I wanted to write a little comment to support you. http://www.kayswell.com
You’re so interesting! I don’t suppose I have read something like this before. So nice to discover another person with a few genuine thoughts on this subject. Seriously.. many thanks for starting this up. This web site is something that’s needed on the web, someone with a little originality! http://www.kayswell.com
I really like what you guys tend to be up too. This kind of clever work and reporting! Keep up the amazing works guys I’ve added you guys to my blogroll. http://www.kayswell.com
Heya this is kinda of off topic but I was wanting to know if blogs use WYSIWYG editors or if you have to manually code with HTML. I’m starting a blog soon but have no coding know-how so I wanted to get guidance from someone with experience. Any help would be enormously appreciated! http://www.kayswell.com
First off I would like to say superb blog! I had a quick question which I’d like to ask if you don’t mind. I was interested to find out how you center yourself and clear your thoughts before writing. http://www.kayswell.com I have had a difficult time clearing my mind in getting my ideas out there.I truly do take pleasure in writing but it just seems like the first 10 to 15 minutes are
Aw, this was a very nice post. Taking the time and actual effort to create a great article… but what can I say… I hesitate a whole lot and never seem to get nearly anything done. http://www.kayswell.com
I loved as much as you will receive carried out right here. The sketch is tasteful, your authored material stylish. nonetheless, you command get bought an edginess over that you wish be delivering the following. http://www.kayswell.com unwell unquestionably come further formerly again since exactly the same nearly very often inside case you shield this hike.
Do you mind if I quote a few of your articles as long as I provide credit and sources back to your website? My website is in the exact same area of interest as yours and my visitors would definitely benefit from some of the information you provide here. http://www.kayswell.com
Heya i am for the first time here. I found this board and I to find It truly helpful & it helped me out much. I hope to offer one thing back and help others like you aided me. http://www.kayswell.com
You’re so interesting! I don’t suppose I have read something like this before. So nice to discover another person with a few genuine thoughts on this subject. Seriously.. many thanks for starting this up. This web site is something that’s needed on the web, someone with a little originality! http://www.kayswell.com
Hi there, everything is going sound here and ofcourse every one is sharing data, that’s really good, keep up writing. http://www.kayswell.com
I’m really enjoying the design and layout of your website.It’s a very easy on the eyes which makes it much more pleasant for me to come here and visit more often. Did you hire out a developer to create your theme? http://www.kayswell.com
Thanks for your help and for writing this post. It’s been great. http://www.kayswell.com
I’d like to thank you for the efforts you have put in writing this blog.I’m hoping to check out the same high-grade content from you later on as well. In truth, http://www.kayswell.com your creative writing abilities has motivated me to get my very own website now 😉
Your mode of explaining everything in this piece of writing is genuinely pleasant, every one be capable of simply be aware of it, Thanks a lot. http://www.kayswell.com
Hey there! Would you mind if I share your blog with my myspace group? There’s a lot of people that I think would really enjoy your content. Please let me know. Thanks
What’s Happening i’m new to this, I stumbled upon this I have found It positively useful and it has helped me out loads. I hope to contribute & assist other users like its aided me. Great job.
I loved as much as you will receive carried out right here. The sketch is tasteful, your authored material stylish. nonetheless, you command get bought an edginess over that you wish be delivering the following. unwell unquestionably come further formerly again since exactly the same nearly very often inside case you shield this hike.
I think the admin of this website is in fact working hard in support of his website, as here every stuff is quality based stuff.
We’re a group of volunteers and starting a new scheme in our community. Your website offered us with helpful information to work on. You’ve done a formidable task and our whole community will be thankful to you.
What i don’t realize is in truth how you’re no longer actually a lot more neatly-preferred than you might be now. You’re so intelligent. You know therefore considerably relating to this topic, produced me personally imagine it from numerous varied angles. Its like men and women aren’t interested except it抯 one thing to do with Girl gaga! Your own stuffs great. At all times maintain it up!
Simply want to say your article is as astonishing. The clarity for your post is just excellent and i can think you are knowledgeable in this subject. Fine with your permission allow me to clutch your feed to keep updated with forthcoming post. Thanks a million and please carry on the gratifying work.
Hmm is anyone else having problems with the pictures on this blog loading? I’m trying to determine if its a problem on my end or if it’s the blog. Any suggestions would be greatly appreciated.
Greetings! Very helpful advice in this particular article! It’s the little changes that will make the most significant changes. Thanks a lot for sharing!
I really like your writing style, good info , appreciate it for posting : D.
Hey there! Would you mind if I share your blog with my myspace group? There’s a lot of people that I think would really enjoy your content. Please let me know. Thanks http://www.kayswell.com
Hello to all, the contents existing at this web page are genuinely remarkable for people knowledge, well, keep up the good work fellows. http://www.kayswell.com
What’s Going down i’m new to this, I stumbled upon this I have discovered It absolutely useful and it has aided me out loads. I am hoping to give a contribution & assist other users like its helped me. Great job.
Do you mind if I quote a few of your articles as long as I provide credit and sources back to your website? My blog site is in the exact same area of interest as yours and my visitors would really benefit from a lot of the information you provide here.Please let me know if this ok with you. Regards!
I like reading through and I conceive this website got some truly utilitarian stuff on it! .
If some one needs to be updated with latest technologies therefore he must be go to see this web site and be up to date every day.
It’s a pity you don’t have a donate button! I’d definitely donate to this fantastic blog! I guess for now i’ll settle for bookmarking and adding your RSS feed to my Google account. I look forward to new updates and will share this blog with my Facebook group. Talk soon!
Pretty great post. I just stumbled upon your weblog and wanted to say that I have really loved browsing your weblog posts. After all I’ll be subscribing on your feed and I hope you write once more very soon! http://www.kayswell.com
Hello there, You’ve done a great job. I will definitely digg it and personally recommend to my friends. I am confident they will be benefited from this website. http://www.kayswell.com
Oh my goodness! Amazing article dude! Many thanks, However I am encountering problems with your RSS. I don’t understand the reason why I can’t join it. Is there anybody else having similar RSS issues? Anyone who knows the answer can you kindly respond? http://www.kayswell.com
Ahaa, its good dialogue regarding this article at this place at this website, I have read all that, so at this time me also commenting here.
I’m not that much of a internet reader to be honest but your blogs really nice, keep it up! I’ll go ahead and bookmark your site to come back down the road. Many thanks
This is my first time pay a visit at here and i am really pleassant to read all at single place. http://www.kayswell.com
This paragraph will assist the internet users for building up new web site or even a blog from start to end. http://www.ifashionstyles.com
When someone writes an piece of writing he/she keeps the thought of a user in his/her brain that how a user can know it. So that’s why this paragraph is outstdanding.
This is a topic that’s near to my heart… Many thanks! Where are your contact details though?
I am regular reader, how are you everybody? This post posted at this web page is genuinely pleasant.
Hi there, just became alert to your blog through Google,and found that it is truly informative. I am gonna watch outfor brussels. I’ll be grateful if you continue this in future.Lots of people will be benefited from your writing.Cheers! http://www.kayswell.com
I’m not that much of a internet reader to be honest but your blogs really nice, keep it up! I’ll go ahead and bookmark your website to come back in the future. http://www.hairstylesvip.com
Greetings! Very helpful advice in this particular article! It’s the little changes that will make the most significant changes. Thanks a lot for sharing!
Hurrah! In the end I got a weblog from where I know how to truly take helpful information regarding my study and knowledge.
I think what you typed was very logical. However, what about this?
suppose you were to write a killer headline? I mean, I don’t wish to
tell you how to run your blog, however what if you added a post title to possibly get
folk’s attention? I mean Top 20 Fast-Acting Painkillers For Quick
And Effective Relief – Welcome To Healoopedia is
kinda boring. You should peek at Yahoo’s home page and see
how they create article titles to grab viewers to click.
You might add a related video or a related pic or two to grab readers interested about everything’ve got to
say. Just my opinion, it would make your posts a little bit more interesting.
I?¦m now not sure where you are getting your info, however great topic. I must spend some time studying more or understanding more. Thanks for wonderful info I used to be on the lookout for this information for my mission.
If some one needs to be updated with latest technologies therefore he must be go to see this web site and be up to date every day.
Now I am ready to do my breakfast, once having my breakfast coming over again to read more news http://www.kayswell.com
This is my first time pay a visit at here and i am really pleassant to read all at single place. http://www.ifashionstyles.com
I think that is one of the most significant info for me. And i am glad studying your article. However should statement on some basic issues, The site style is perfect, the articles is actually nice : D. Just right activity, cheers
We’re a group of volunteers and starting a new scheme in our community. Your website offered us with helpful information to work on. You’ve done a formidable task and our whole community will be thankful to you. http://www.ifashionstyles.com
If you would like to obtain a great deal from this paragraph then you have to apply these methods to your won website. http://www.hairstylesvip.com
What’s up i am kavin, its my first time to commenting anywhere, when i read this paragraph i thought i could also make comment due to this sensible post. http://www.hairstylesvip.com
to this require a great deal of work? I have very little knowledge of computer programming however I had been hoping to start my own blog in the near future. Anyway, should you have any suggestions or tips for new blog owners please share. I understand this is off topic but I simply needed to ask.
Hello mates, its wonderful post on the topic of cultureand entirely explained, keep it up all the time.
Really when someone doesn’t be aware of afterward its up to other viewers that they will help, so here it occurs.
I know this if off topic but I’m looking into starting my own blog and was curious what all is needed to get setup? I’m assuming having a blog like yours would cost a pretty penny? http://www.ifashionstyles.com I’m not very web savvy so I’m not 100 sure. Any recommendations or advice would be greatly appreciated. Thanks
Thank you for the auspicious writeup. It in fact was a amusement account it. Look advanced to far added agreeable from you! By the way, how could we communicate? http://www.kayswell.com
You should be a part of a contest for one of the finest blogs on the net. I’m going to highly recommend this blog! http://www.kayswell.com
Hello very nice web site!! Man .. Beautiful .. Amazing .. I will bookmark your site and take the feeds also? I am satisfied to seek out so many useful information here in the put up, we want work out extra techniques on this regard, thank you for sharing. http://www.kayswell.com
Hello there, You’ve done a great job. I will certainly digg it and personally recommend to my friends. I’m sure they will be benefited from this site.
What’s up, after reading this awesome post i am too happy to share my familiarity here with colleagues.
When I initially commented I clicked the “Notify me when new comments are added” checkbox and now each time a comment is added I get several emails with the same comment. Is there any way you can remove people from that service? Many thanks!
Nice answers in return of this matter with firm arguments and telling everything concerning that.
Hello There. I found your blog using msn. This is a really well written article. I will be sure to bookmark it and come back to read more of your useful information. Thanks for the post. I’ll certainly return.
First off I would like to say superb blog! I had a quick question which I’d like to ask if you don’t mind. I was interested to find out how you center yourself and clear your thoughts before writing. http://www.kayswell.com I have had a difficult time clearing my mind in getting my ideas out there.I truly do take pleasure in writing but it just seems like the first 10 to 15 minutes are
I have acquired some new elements from your web page about desktops. Another thing I’ve always presumed is that computers have become a product that each family must have for some reasons. They supply you with convenient ways in which to organize the home, pay bills, go shopping, study, pay attention to music and perhaps watch tv shows. An innovative approach to complete all of these tasks is a laptop computer. These personal computers are mobile ones, small, highly effective and transportable.
Hello colleagues, its enormous article regarding cultureand completely defined, keep it up all the time. http://www.kayswell.com
I’ve been surfing online more than 3 hours today, yet I never found any interesting article like yours. It’s pretty worth enough for me. Personally, if all webmasters and bloggers made good content as you did, the web will be much more useful than ever before.
If some one desires expert view concerning blogging afterward i advise him/her to pay a visit this weblog, Keep up the good work. http://www.hairstylesvip.com
Valuable information. Lucky me I found your website by accident, and I am shocked why this accident did not happened earlier! I bookmarked it.
Its like you read my mind! You seem to know a lot about this, like you wrote the book in it or something. I think that you could do with a few pics to drive the message home a little bit, but other than that, this is excellent blog. A fantastic read. I’ll definitely be back.
This is my first time pay a visit at here and i am really pleassant to read all at single place. http://www.hairstylesvip.com
One more issue is really that video gaming became one of the all-time biggest forms of excitement for people of nearly every age. Kids engage in video games, and also adults do, too. Your XBox 360 is one of the favorite video games systems for those who love to have hundreds of video games available to them, plus who like to relax and play live with other folks all over the world. Thank you for sharing your notions.
Hi every one, here every person is sharing these kinds of knowledge, therefore it’s good to read this blog, and I used to pay a quick visit this blog daily.
Spot on with this write-up, I really believe this site needs much more attention. I’ll probably be returning to read through more, thanks for the info!
Hey there! Would you mind if I share your blog with my myspace group? There’s a lot of people that I think would really enjoy your content. Please let me know. Thanks
Touche. Outstanding arguments. Keep up the great work. http://www.hairstylesvip.com
I am curious to find out what blog platform you happen to be utilizing? I’m experiencing some minor security issues with my latest blog and I would like to find something more safeguarded. Do you have any suggestions? http://www.hairstylesvip.com
What a information of un-ambiguity and preserveness of valuable familiarity on the topic of unexpected feelings.
I simply wanted to thank you very much again. I do not know what I would’ve taken care of without the type of advice revealed by you directly on such situation. It had become the frustrating crisis in my view, but encountering this specialized manner you handled it made me to jump for delight. Now i am happier for your work and in addition pray you are aware of a powerful job you’re providing instructing people thru a web site. Most probably you haven’t got to know any of us.
generally lost just trying to figure out how to begin. Any ideas or tips?
I love the efforts you have put in this, thanks for all the great content.
You should be a part of a contest for one of the finest blogs on the net. I’m going to highly recommend this blog!
Hurrah! In the end I got a weblog from where I know how to truly take helpful information regarding my study and knowledge.
Thanks for another excellent post. Where else could anyone get that kind of info in such an ideal way of writing? I’ve a presentation next week, and I’m on the look for such info.
Downloading games from 92rgamedownload is surprisingly easy. The selection is decent, and the downloads are fast. A solid choice for finding new games. Give it a try here: 92rgamedownload
I am really loving the theme/design of your weblog. Do you ever run into any browser compatibility issues? A few of my blog readers have complained about my site not working correctly in Explorer but looks great in Firefox. Do you have any advice to help fix this issue? http://www.kayswell.com